A cervical radiofrequency ablation (RFA) is an outpatient procedure for treating low back, buttock, hip, and groin pain. It is also called cervical facet denervation, neurotomy or rhizotomy.
You may feel pain if a cervical facet joint is injured. Sometimes it feels like muscle tension, a constant ache which worsens with movements. Its usually described as a pain in the lower part of the neck and across the shoulders. Some patients are also troubled with headaches. With worsening pain from the cervical facets, the pain may travel down the limbs. Ongoing pain may result in weakening of the adjoining muscles and ligaments.
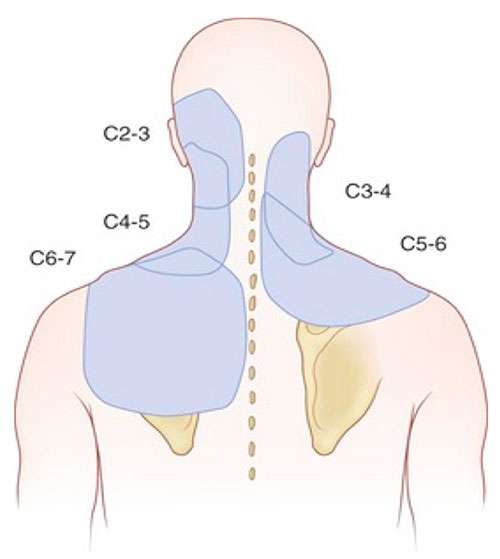
Facet pain also depends on which joint is affected. Cervical facet joint pain can occur in an area from your neck, shoulders and head. The diagram shows areas of pain usually associated with cervical facet injuries.
If you have pain in one or more of these areas shown in the diagram, and it has lasted longer than 3 months you may have cervical facet pain. Common tests such as x-rays or MRIs may not always show if a facet joint is causing pain. The best way to diagnose facet pain is to block the pain signal in a medial branch nerve with a local anaesthetic (numbing medicine).

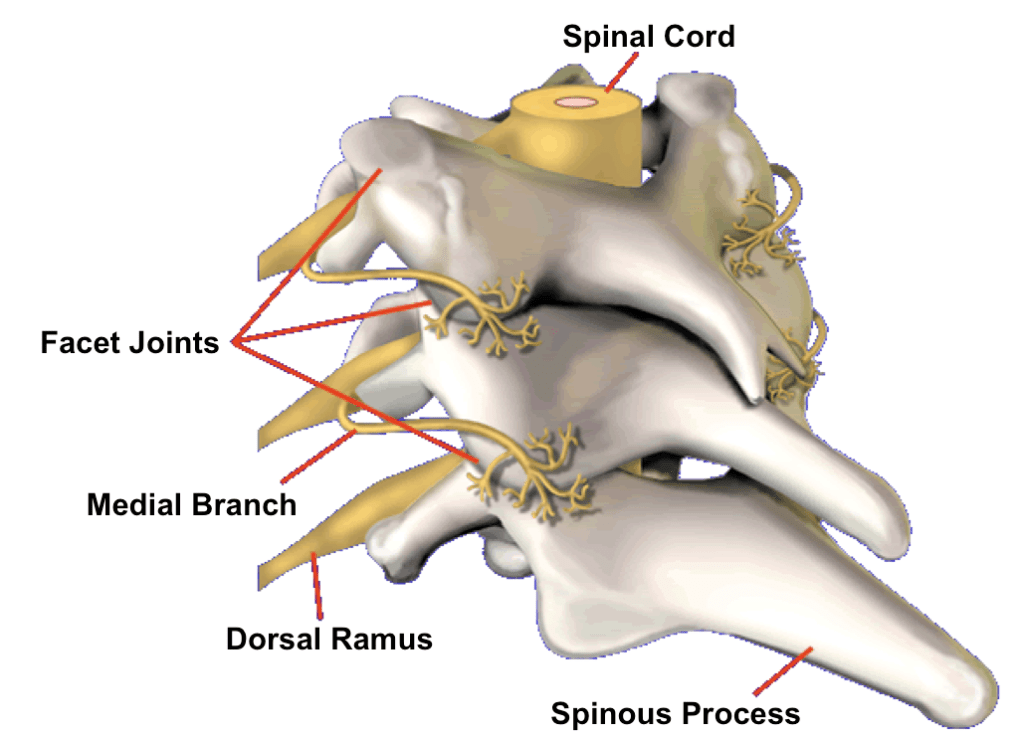
RFA uses radiofrequency energy to disrupt nerve function. When this is done to a cervical medial branch nerve, the nerve can no longer transmit pain from an injured facet joint.
The procedure is performed in the operation theatre. You will be sedated and local anaesthesia will be used to numb your skin. The doctor will then insert a small needle near the Cervical medial branch nerve. Fluoroscopy, a type of x-ray, will be used to ensure the safe and proper position of the needle. Once the doctor is sure the needle is correctly placed, the medicine will be injected. Radiofrequency energy will then be used to disrupt the medial branch nerve. This is often repeated at more than one level of the spine.
You will be monitored for up to monitored closely in the recovery room for 30 minutes after the injection. When you are ready to leave, the staff will give you discharge instructions. You will need to keep a pain diary. It is important to maintain a diary to help the doctor ascertain the success of the RFA.
You may feel sore for one to four days. It may be due to muscle and nerve irritation. Your back may feel numb, weak, or itchy for a couple weeks. Maximum pain relief normally comes in two to three weeks, but can take as long as six to eight weeks.
Nerves regenerate after an RFA, but how long this takes varies. Your pain may or may not return when the nerves regenerate which can range from 9 to 18 months. If it does, another RFA can be done.
Please advise staff if you are:
Operating department staff may advise you to:
Contact us, your GP or Local Emergency department , if you experience the following:
This pamphlet is for general education only. Specific questions or concerns should always be directed to your doctor. Your doctor can explain possible risks or side effects.
©2025 PainMed. All Rights Reserved. Website Developed by Clickmatix
Originally from England, Sally graduated from St George’s Hospital, University of London in 2004 with a BSc (First Class Hons) in Physiotherapy. Since settling in Australia, Sally has worked in private practice and in the public hospital setting across Sydney.
Sally gained a Masters in Medicine Pain Management from the University of Sydney in 2019 and is a Titled Pain Physiotherapist (as awarded by the Australian Physiotherapy Association).
In addition to private practice, Sally currently works as a Senior Physiotherapist at Westmead Hospital Pain Management Service.
Sally is highly skilled in assessing, diagnosing and treating people who experience chronic pain. She enjoys working with injured workers and CTP claimants. She has a deep understanding of the impact of pain on the whole person and on their functioning in daily life. In partnership with her colleagues, Sally enjoys applying her knowledge and clinical skills to provide a safe space for exploration of the physical and emotional meaning of pain and for recovery of function.
Qualifications and Experience
Dr. Adam is a Fellowship-trained Pain Medicine Specialist with a Fellowship from the Faculty of Pain Medicine (FFPMANZCA) and a Master of Pain Medicine from the University of Sydney. He is dedicated to the comprehensive management of chronic pain across all age groups.
Dr. Adam trained in adult pain medicine at Liverpool Hospital, Nepean Hospital, and the Department of Pain Medicine, and completed additional training in paediatric chronic pain at The Children’s Hospital at Westmead. He currently serves as a Staff Specialist at Westmead and St George Public Hospitals (NSW Health), and is a Visiting Medical Officer (VMO) at Liverpool Public Hospital, St George Private, Sydney Southwest Private, Holroyd Private, Norwest Private, and Nepean Private Hospitals.
He adopts a whole-person, multidisciplinary approach rooted in the socio-psycho-biomedical model, utilising both pharmacologic and interventional techniques. These include:
Dr. Adam is an Authorised Prescriber of Medicinal Cannabis and holds a Diploma in Medicinal Cannabis. He is also certified in Opioid Treatment Programs, including Methadone, Suboxone, and Buprenorphine injections. His areas of interest include opioid dependence management, medicinal cannabis, and interventional pain procedures.
He also completed advanced training in Virtual Reality Therapy for chronic pain and mental health disorders in Barcelona, Spain, and has further qualifications in Focused Psychological Strategies, Cognitive Behavioural Therapy (CBT), and Clinical Hypnosis.
Qualifications: