Thoracic Radiofrequency Ablation
A thoracic radiofrequency ablation (RFA) is an outpatient procedure for treating low back, buttock, hip, and groin pain. It is also called thoracic facet denervation, neurotomy or rhizotomy.
What are Thoracic Facet Joints?
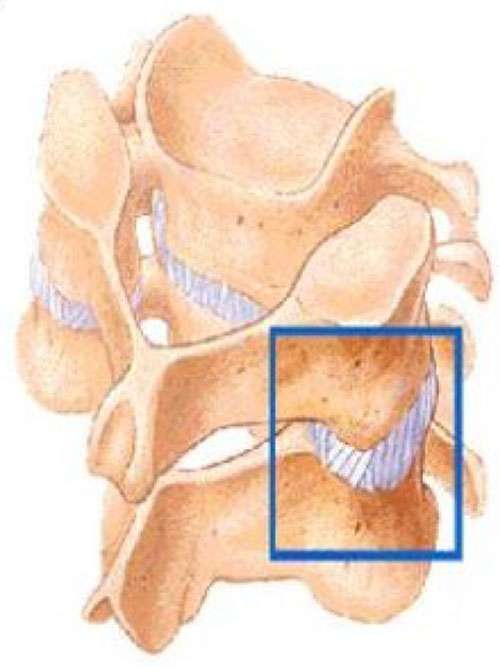
Facet joints (also called zygapophyseal joints) are small joints of the spine that provide stability and help guide motion. They are found in the neck (lumbar), upper back (thoracic) and lower back (lumbar). They can become painful as a result of arthritis, injury or mechanical stress. Two nerves called “medial branches” supply each facet joint. These nerves carry pain signals to the spinal cord and these signals will eventually reach the brain. The proportion of patients who are affected by facet related pain increased with age and can be as high as 45% in patient population with spinal pain.
What is thoracic facet joint pain?
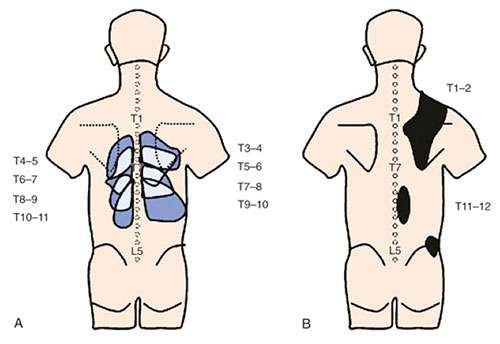
You may feel pain if a thoracic facet joint is injured. Sometimes it feels like muscle tension, a constant ache which worsens with movements. Its usually described as a pain in the upper back fairly localised to the area. With worsening pain from the thoracic facets, the pain may travel along the spine and around the chest wall like a corset. Ongoing pain may result in weakening of the adjoining muscles and ligaments.
Facet pain also depends on which joint is affected. Thoracic facet joint pain can occur in an area from your upper back and the chest wall. The diagram shows areas of pain usually associated with thoracic facet injuries.
 How do I know if I have thoracic facet pain?
How do I know if I have thoracic facet pain?
If you have pain in one or more of these areas shown in the diagram, and it has lasted longer than 3 months you may have thoracic facet pain. Common tests such as x-rays or MRIs may not always show if a facet joint is causing pain. The best way to diagnose facet pain is to block the pain signal in a medial branch nerve with a local anaesthetic (numbing medicine).
What is a thoracic RFA?
RFA uses radiofrequency energy to disrupt nerve function. When this is done to a thoracic medial branch nerve, the nerve can no longer transmit pain from an injured facet joint.
What happens during an RFA?
The procedure is performed in the operation theatre. You will be sedated and local anaesthesia will be used to numb your skin. The doctor will then insert a small needle near the Thoracic medial branch nerve. Fluoroscopy, a type of x-ray, will be used to ensure the safe and proper position of the needle. Once the doctor is sure the needle is correctly placed, the medicine will be injected. Radiofrequency energy will then be used to disrupt the medial branch nerve. This is often repeated at more than one level of the spine.
What happens after an RFA?
You will be monitored for up to monitored closely in the recovery room for 30 minutes after the injection. When you are ready to leave, the staff will give you discharge instructions. You will need to keep a pain diary. It is important to maintain a diary to help the doctor ascertain the success of the RFA.
You may feel sore for one to four days. It may be due to muscle and nerve irritation. Your back may feel numb, weak, or itchy for a couple weeks. Maximum pain relief normally comes in two to three weeks, but can take as long as six to eight weeks.
How long can I expect pain relief?
Nerves regenerate after an RFA, but how long this takes varies. Your pain may or may not return when the nerves regenerate which can range from 9 to 18 months. If it does, another RFA can be done.
How do I prepare for the procedure?
Please advise staff if you are:
- Taking blood thinners (especially warfarin and clopidogrel)
- Diabetic
- Pregnant (or any chance of you being pregnant).
- Allergic to iodine, betadine, shellfish, local anaesthetics, or steroids.
- Unwell (especially if you have an infection)
Operating department staff may advise you to:
- Fast
- Take your usual medications (apart from those mentioned above)
- Arrange for someone to accompany you home
When do I seek medical attention after the procedure?
Contact us, your GP or Local Emergency department , if you experience the following:
- Loss of bowel or bladder control
- Weakness in your limbs
- Fever: temperature above 38℃ that does not improve
This pamphlet is for general education only. Specific questions or concerns should always be directed to your doctor. Your doctor can explain possible risks or side effects.



